Difference between revisions of "AY Honors/First Aid/Answer Key/es"
(Created page with "</noinclude> <!-- 26. Conocer los primeros auxilios adecuados para las picaduras de garrapatas. -->") |
(Updating to match new version of source page) |
||
| Line 40: | Line 40: | ||
<noinclude></noinclude> | <noinclude></noinclude> | ||
<!-- 5. Conocer la información de contacto para emergencias en el área donde vive. Hacer una lista de la información necesaria para contactarse con ellos en caso de emergencia. Ver un video educativo acerca de cómo comunicarse con los servicios de emergencia o entrevistar a un paramédico o a un operador de servicios de emergencia médica. --> | <!-- 5. Conocer la información de contacto para emergencias en el área donde vive. Hacer una lista de la información necesaria para contactarse con ellos en caso de emergencia. Ver un video educativo acerca de cómo comunicarse con los servicios de emergencia o entrevistar a un paramédico o a un operador de servicios de emergencia médica. --> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | In most states in the U.S., it is 9-1-1. When calling in, you need to provide information on the emergency which includes the following: | ||
| + | * Location, address or area identifying information. | ||
| + | * Number of victims, Injury or illness that you can observe, and the operator may ask for other specific information. | ||
| + | </div> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | Contact 9-1-1 (Emergency phone number for the United States –(KNOW YOUR emergency contact information where you are located) - provide information on your particular emergency, i.e., location, number of victims, injury or illness that you are observing, etc. If you are alone, you may need to contact 9- 1-1 first. If you can summon others to help, one may be able to phone 9-1-1 and relay messages. If you are alone, without a cell phone, shout for help. | ||
| + | </div> | ||
<noinclude></noinclude> | <noinclude></noinclude> | ||
| Line 153: | Line 163: | ||
<noinclude></noinclude> | <noinclude></noinclude> | ||
<!-- 16. Saber cuándo y cómo utilizar correctamente un torniquete. Utilizando un gráfico, un maniquí u otro dispositivo de instrucción, demostrar dónde se encuentran los distintos puntos de presión en un cuerpo y cómo aplicar la presión correctamente. --> | <!-- 16. Saber cuándo y cómo utilizar correctamente un torniquete. Utilizando un gráfico, un maniquí u otro dispositivo de instrucción, demostrar dónde se encuentran los distintos puntos de presión en un cuerpo y cómo aplicar la presión correctamente. --> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | A '''tourniquet''' is a tightly tied band applied around a body part (an arm or a leg) sometimes used in an attempt to stop severe traumatic bleeding. Severe bleeding means the loss of more than 1,000 ml (1 litre) of blood. This flow of blood can soak a paper or cloth handkerchief in a few seconds. In such a situation, the bleeding will cause the death of the casualty in seconds to minutes. | ||
| + | </div> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | A tourniquet is a ''last resort'' method of bleeding control. Other methods that should be applied first and in conjunction, if possible, include: | ||
| + | </div> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | * direct pressure | ||
| + | * elevation of the limb or wound above the heart | ||
| + | * the use of a pressure point to slow the artery above the injury(s) | ||
| + | * blood-clotting agents or bandages | ||
| + | </div> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | Even in cases of amputation, most bleeding can be controlled through these alternative methods. The rare exception is when a limb is shattered by massive trauma or when a major blood vessel is torn along its length. Even in these cases, the use of a pressure point above the wound is strongly preferred. | ||
| + | </div> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | As the tourniquet stops blood flow to the limb, it can cause the death of the limb, forcing the later surgical amputation of the limb just below the level the tourniquet is applied. This is likely to occur when the tourniquet stays in place several hours. In any event, once a tourniquet has been applied, advanced medical care from a doctor or hospital ''will'' be required to salvage the limb if not save the life of the patient. | ||
| + | </div> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | The decision to employ a tourniquet should be made by an emergency medical technician or preferably a doctor if at all possible. But when severe external bleeding cannot be controlled by other means, a tourniquet may be the only way for a first-aider to save the casualty. | ||
| + | </div> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | Most civilian first aid instruction in the United States no longer teaches the use of the tourniquet for the following reasons: | ||
| + | * the effectiveness of direct pressure, elevation and pressure points (controlling severe bleeding in up to 90% of cases as estimated by US medical sources) | ||
| + | * the increased difficulty of reattaching an amputated limb when a tourniquet has been applied to the victim | ||
| + | * unnecessary use by poorly trained bystanders | ||
| + | * the unavoidable risks to both limb and life even when properly employed | ||
| + | * the rare nature of injuries that require tourniquets, which typically occur in unusual settings such as working with agricultural or industrial machinery and the battlefield | ||
| + | </div> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | The use of a tourniquet by a layperson in countries where it is considered outside the scope of practice of first aid may result in civil lawsuits and/or criminal charges, especially if the application was later found to have been unnecessary. | ||
| + | </div> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | {{:AY Honors/First aid/Pressure_points}} | ||
| + | </div> | ||
<noinclude></noinclude> | <noinclude></noinclude> | ||
| Line 231: | Line 285: | ||
{{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=23b}} | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=23b}} | ||
<noinclude></noinclude> | <noinclude></noinclude> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | The figure-eight bandage can also be used on the hand, wrist, elbow, and knee. | ||
| + | </div> | ||
<noinclude></noinclude> | <noinclude></noinclude> | ||
| Line 258: | Line 316: | ||
<noinclude></noinclude> | <noinclude></noinclude> | ||
{{CloseReq}} <!-- 23f --> | {{CloseReq}} <!-- 23f --> | ||
| + | {{:AY Honors/First aid/Forearm_splint}} | ||
{{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=23g}} | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=23g}} | ||
| Line 264: | Line 323: | ||
<noinclude></noinclude> | <noinclude></noinclude> | ||
{{CloseReq}} <!-- 23g --> | {{CloseReq}} <!-- 23g --> | ||
| + | {{:AY Honors/First aid/Ankle_splint}} | ||
{{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=23h}} | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=23h}} | ||
| Line 275: | Line 335: | ||
<noinclude></noinclude> | <noinclude></noinclude> | ||
<!-- 24. Describir el tratamiento adecuado para las lesiones por quemaduras y las lesiones eléctricas. --> | <!-- 24. Describir el tratamiento adecuado para las lesiones por quemaduras y las lesiones eléctricas. --> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | For chemical burns: | ||
| + | {{:AY Honors/First aid/Chemical_burn}} | ||
| + | </div> | ||
<noinclude></noinclude> | <noinclude></noinclude> | ||
| Line 296: | Line 361: | ||
<noinclude></noinclude> | <noinclude></noinclude> | ||
<!-- 27. Discutir con su instructor cómo reconocer los síntomas de las emergencias relacionadas con el calor y las emergencias relacionadas con el frío. Conocer y demostrar las respuestas adecuadas para cada una de ellas. --> | <!-- 27. Discutir con su instructor cómo reconocer los síntomas de las emergencias relacionadas con el calor y las emergencias relacionadas con el frío. Conocer y demostrar las respuestas adecuadas para cada una de ellas. --> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | '''Heat Exhaustion''' | ||
| + | {{:AY Honors/First aid/Heat exhaustion}} | ||
| + | </div> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | '''Hypothermia''' | ||
| + | {{:AY Honors/First aid/Hypothermia}} | ||
| + | </div> | ||
| + | |||
| + | <div lang="en" dir="ltr" class="mw-content-ltr"> | ||
| + | '''Frostbite''' | ||
| + | {{:AY Honors/First aid/Frostbite}} | ||
| + | </div> | ||
<noinclude></noinclude> | <noinclude></noinclude> | ||
Revision as of 15:09, 5 October 2023
Nivel de destreza
2
Año
1938
Version
06.02.2026
Autoridad de aprobación
División Norteamericana
Instructor requerido
1
Completar el requisito 2 Ó 3-29.
2
3
4
5
In most states in the U.S., it is 9-1-1. When calling in, you need to provide information on the emergency which includes the following:
- Location, address or area identifying information.
- Number of victims, Injury or illness that you can observe, and the operator may ask for other specific information.
Contact 9-1-1 (Emergency phone number for the United States –(KNOW YOUR emergency contact information where you are located) - provide information on your particular emergency, i.e., location, number of victims, injury or illness that you are observing, etc. If you are alone, you may need to contact 9- 1-1 first. If you can summon others to help, one may be able to phone 9-1-1 and relay messages. If you are alone, without a cell phone, shout for help.
6
- La víctima no responde a la voz ni al tacto
- Confusión, nivel de conciencia
- Malestar en el pecho, posible ataque cardiaco
- Signos de derrame cerebral
- Problemas respiratorios
- Lesión o quemadura grave
- Hemorragia grave
- Convulsión
- Parálisis
- Envenenamiento de una parte del cuerpo
- Choque eléctrico
7
7a
7b
7c
8
8a
8b
8c
9
10
11
12
13
14
15
16
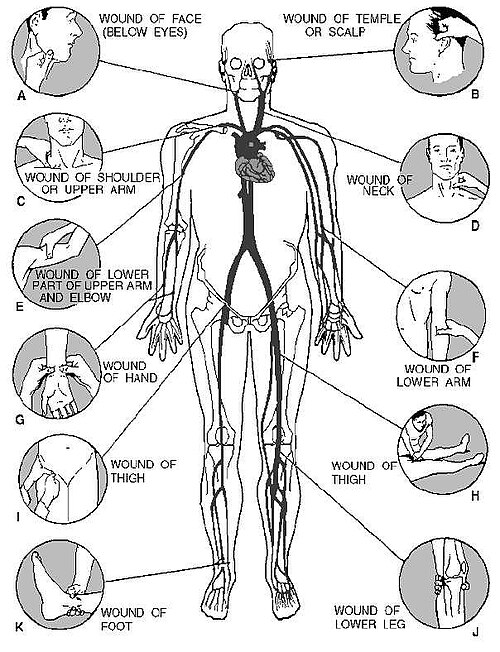
A tourniquet is a tightly tied band applied around a body part (an arm or a leg) sometimes used in an attempt to stop severe traumatic bleeding. Severe bleeding means the loss of more than 1,000 ml (1 litre) of blood. This flow of blood can soak a paper or cloth handkerchief in a few seconds. In such a situation, the bleeding will cause the death of the casualty in seconds to minutes.
A tourniquet is a last resort method of bleeding control. Other methods that should be applied first and in conjunction, if possible, include:
- direct pressure
- elevation of the limb or wound above the heart
- the use of a pressure point to slow the artery above the injury(s)
- blood-clotting agents or bandages
Even in cases of amputation, most bleeding can be controlled through these alternative methods. The rare exception is when a limb is shattered by massive trauma or when a major blood vessel is torn along its length. Even in these cases, the use of a pressure point above the wound is strongly preferred.
As the tourniquet stops blood flow to the limb, it can cause the death of the limb, forcing the later surgical amputation of the limb just below the level the tourniquet is applied. This is likely to occur when the tourniquet stays in place several hours. In any event, once a tourniquet has been applied, advanced medical care from a doctor or hospital will be required to salvage the limb if not save the life of the patient.
The decision to employ a tourniquet should be made by an emergency medical technician or preferably a doctor if at all possible. But when severe external bleeding cannot be controlled by other means, a tourniquet may be the only way for a first-aider to save the casualty.
Most civilian first aid instruction in the United States no longer teaches the use of the tourniquet for the following reasons:
- the effectiveness of direct pressure, elevation and pressure points (controlling severe bleeding in up to 90% of cases as estimated by US medical sources)
- the increased difficulty of reattaching an amputated limb when a tourniquet has been applied to the victim
- unnecessary use by poorly trained bystanders
- the unavoidable risks to both limb and life even when properly employed
- the rare nature of injuries that require tourniquets, which typically occur in unusual settings such as working with agricultural or industrial machinery and the battlefield
The use of a tourniquet by a layperson in countries where it is considered outside the scope of practice of first aid may result in civil lawsuits and/or criminal charges, especially if the application was later found to have been unnecessary.
The usual way to control bleeding is to put pressure directly onto the wound, either with the hand directly or with a dressing of some sort (bandage, handkerchief, tea towel etc.). Do not forget that any wound which is not controlled within a minute or two is a medical emergency; and any deep or large wound must receive medical attention as soon as possible.
It is sometimes not possible to press directly on a wound: for example, there may be a foreign object inside the wound, or a broken bone protruding outside, or the wound may be too large or be inaccessible (e.g. if the limb is trapped by some immovable object). In this case, the only way to control the bleeding is to compress blood vessels over particular pressure points (usually where arteries cross over bones near to the surface of the skin). This technique can be used to control external bleeding from arm wounds and leg wounds.
The correct point is determined by finding a pulse on a victim similar to that felt in the wrist when taking one's own pulse. This point could be located in the wrist, the arm (on the soft underside of the elbow), the groin, or behind the knee. This is the position where a rhythmical pulsation can be felt. Pressure can then be applied over this point -- the artery -- to control bleeding.
Once an artery is compressed over a pressure point, it must not be compressed for more than 10 minutes: any longer in one go can cause irreversible damage to the limb. Typically pressure would be applied for 10 minutes, then released for a couple, then reapplied and so on.
17
18
18a
18b
18c
19
20
21
22
23
23a
23b
The figure-eight bandage can also be used on the hand, wrist, elbow, and knee.
23c
23d
23e
23f
There are two long bones in the forearm, the radius and the ulna. When both are broken, the arm usually appears to be deformed. When only one is broken, the other acts as a splint and the arm retains a more or less natural appearance. Any fracture of the forearm is likely to result in pain, tenderness, inability to use the forearm, and a kind of wobbly motion at the point of injury. If the fracture is open, a bone will show through. If the fracture is open, stop the bleeding and treat the wound. Apply a sterile dressing over the wound. Carefully straighten the forearm. (Remember that rough handling of a closed fracture may turn it into an open fracture.) Apply two well-padded splints to the forearm, one on the top and one on the bottom. Be sure that the splints are long enough to extend from the elbow to the wrist. Use bandages to hold the splints in place. Put the forearm across the chest. The palm of the hand should be turned in, with the thumb pointing upward. Support the forearm in this position by means of a wide sling and a cravat bandage (see illustration). The hand should be raised about 4 inches above the level of the elbow. Treat the victim for shock and evacuate as soon as possible.
23g
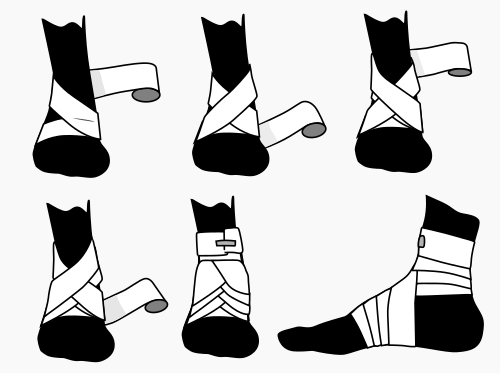
The figure-eight bandage is used for dressings of the ankle, as well as for supporting a sprain. While keeping the foot at a right angle, start a 3-inch bandage around the instep for several turns to anchor it. Carry the bandage upward over the instep and around behind the ankle, forward, and again across the instep and down under the arch, thus completing one figure-eight. Continue the figure-eight turns, overlapping one-third to one-half the width of the bandage and with an occasional turn around the ankle, until the compress is secured or until adequate support is obtained.
23h
24
For chemical burns:
1. For wet chemicals, immediately flush the area with large amounts of water, using a shower or hose, if available. Do not apply water too forcefully. Continue to flood the area while the clothing, including shoes and socks, is being removed. Continue to flush with running water for at least 20 minutes.
- For dry chemicals, brush off the chemical, then flush with water as above.
- For acid burns caused by phenol (carbolic acid), wash the affected area with alcohol because phenol is not water soluble; then wash with water. If alcohol is not available, flushing with water is better than no treatment at all.
2. Call an ambulance
25
26
27
Heat Exhaustion
Heat exhaustion is the most common condition caused by working or exercising in hot spaces. Heat exhaustion produces a serious disruption of blood flow to the brain, heart, and lungs. This causes the victim to experience weakness, dizziness, headache, loss of appetite, and nausea.
Signs and symptoms of heat exhaustion are similar to those of shock: the victim will appear ashen gray; the skin will be cold, moist, and clammy; and the pupils of the eyes may be dilated (enlarged). The vital (blood pressure, temperature, pulse, and respiration) signs usually are normal; however, the victim may have a weak pulse together with rapid and shallow breathing.
Body temperature may be below normal. You should treat heat exhaustion victims as if they were in shock. Loosen the clothing, apply cool wet cloths, move the victim to either a cool or an air-conditioned area, and fan the victim. Do not allow the person to become chilled. If the victim is conscious, administer a solution of 1 teaspoon of salt dissolved in a quart of cool water. If the victim vomits, do not give any more fluids. Transport the victim to a medical facility as soon as possible.
Hypothermia
Hypothermia is caused by continued exposure to low or rapidly falling temperatures, cold moisture, snow, or ice. Those exposed to low temperatures for extended periods may suffer ill effects, even if they are well protected by clothing, because cold affects the body systems slowly, almost without notice. As the body cools, there are several stages of progressive discomfort and disability. he first symptom is shivering, which is an attempt to generate heat by repeated contractions of surface muscles. This is followed by a feeling of listlessness, indifference, and drowsiness. Unconsciousness can follow quickly. Shock becomes evident as the victim’s eyes assume a glassy stare, respiration becomes slow and shallow, and the pulse is weak or absent. As the body temperature drops even lower, peripheral circulation decreases and the extremities become susceptible to freezing. Finally, death results as the core temperature of the body approaches 80°F (27°C). The steps for treatment of hypothermia are as follows:
- Carefully observe respiratory effort and heart beat; CPR may be required while the warming process is underway.
- Rewarm the victim as soon as possible. It may be necessary to treat other injuries before the victim can be moved to a warmer place. Severe bleeding must be controlled and fractures splinted over clothing before the victim is moved.
- Replace wet or frozen clothing and remove anything that constricts the victim’s arms, legs, or fingers, interfering with circulation.
- If the victim is inside a warm place and is conscious, the most effective method of warming is immersion in a tub of warm (100° to 105°F or 38° to 41°C) water. The water should be warm to the elbow - never hot. Observe closely for signs of respiratory failure and cardiac arrest (rewarming shock). Rewarming shock can be minimized by warming the body trunk before the limbs to prevent vasodilation in the extremities with subsequent shock due to blood volume shifts.
- If a tub is not available, apply external heat to both sides of the victim. Natural body heat (skin to skin) from two rescuers is the best method. This is called “buddy warming.” If this is not practical, use hot water bottles or an electric rewarming blanket. Do not place the blanket or bottles next to bare skin, however, and be careful to monitor the temperature of the artificial heat source, since the victim is very susceptible to burn injury. Because the victim is unable to generate adequate body heat, placement under a blanket or in a sleeping bag is not sufficient treatment.
- If the victim is conscious, give warm liquids to drink. Never give alcoholic beverages or allow the victim to smoke.
- Dry the victim thoroughly if water is used for rewarming.
- As soon as possible, transfer the victim to a definitive care facility. Be alert for the signs of respiratory and cardiac arrest during transfer, and keep the victim warm.
Frostbite
Frostbite occurs when ice crystals form in the skin or deeper tissues after exposure to a temperature of 32°F (0°C) or lower. Depending upon the temperature, altitude, and wind speed, the exposure time necessary to produce frostbite varies from a few minutes to several hours.
The areas most commonly affected are the face and extremities. The symptoms of frostbite are progressive. Victims generally incur this injury without being acutely aware of it. Initially, the affected skin reddens and there is an uncomfortable coldness. With continued heat loss, there is a numbness of the affected area due to reduced circulation. As ice crystals form, the frozen extremity appears white, yellow-white, or mottled blue-white, and is cold, hard, and insensitive to touch or pressure. Frostbite is classified as superficial or deep, depending on the extent of tissue involvement.
Superficial Frostbite
In superficial frostbite the surface of the skin will feel hard or rubbery, but the underlying tissue will be soft, allowing it to move over bony ridges. On the exposed skin on the neck and face it is common to first notice patches that are white or waxy in appearance. This is evidence that only the skin and the region just below it are involved. Very little information is available in wilderness first aid training on the appearance of mid and dark toned skin that has been exposed to mild or superficial frostbite. General treatment for superficial frostbite is as follows:
- Take the victim indoors, or at a minimum, increase their shelter from the elements.
- Superficial frostbite around the head can typically be reversed quickly by sheltering from the elements with a scarf, hat, or even a gloved hand.
- Rewarm hands by placing them under the armpits, against the abdomen, or between the legs.
- Rewarm feet by placing them in the armpit or against the abdomen of the buddy.
- Gradually rewarm the affected area by warm water immersion, skin-to-skin contact, or hot water bottles.
- Place hot water bottles into a dry sock/glove to avoid overheating skin.
- Never rub a frostbite area.
Deep Frostbite
In deep frostbite, the freezing reaches into the deep tissue layers. There are ice crystals in the entire thickness of the extremity. The skin will not move over bony ridges and will feel hard and solid. The objectives of treatment are to protect the frozen areas from further injury, to rapidly thaw the affected area, and to be prepared to respond to circulatory or respiratory difficulties.
- Carefully assess and treat any other injuries first. Constantly monitor the victim’s pulse and breathing since respiratory and heart problems can develop rapidly. Be prepared to administer CPR if necessary.
- Do not attempt to thaw the frostbitten area if there is a possibility of refreezing. It is better to leave the part frozen until the victim arrives at a medical treatment facility equipped for long-term care. Refreezing of a thawed extremity causes severe and disabling damage.
- Treat all victims with injuries to the feet or legs as litter patients. When this is not possible, the victim may walk on the frozen limb, since it has been proven that walking will not lessen the chances of successful treatment as long as the limb has not thawed out.
- When adequate protection from further cold exposure is available, prepare the victim for rewarming by removing all constricting clothing such as gloves, boots, and socks. Boots and clothing frozen on the body should be thawed by warm-water immersion before removal.
- Rapidly rewarm frozen areas by immersion in water at 100°F to 105°F (38°C to 41°C). Keep the water warm by adding fresh hot water, but do not pour the water directly on the injured area. Ensure that the frozen area is completely surrounded by water; do not let it rest on the side or bottom of the tub.
- After rewarming has been completed, pat the area dry with a soft towel. Later it will swell, sting, and burn. Blisters may develop. These should be protected from breaking. Avoid pressure, rubbing, or constriction of the injured area. Keep the skin dry with sterile dressings and place cotton between the toes and fingers to prevent their sticking together.
- Protect the tissue from additional injury and keep it as clean as possible (use sterile dressings and linen).
- Try to improve the general morale and comfort of the victim by giving hot, stimulating fluids such as tea or coffee. Do not allow the victim to smoke or use alcoholic beverages while being treated.
- Transfer to a medical treatment facility as soon as possible. During transportation, slightly elevate the frostbitten area and keep the victim and the injured area warm. Do not allow the injured area to be exposed to the cold.
28
29
29a
29b
29c
29d
29e
29f
29g
Nota: Ya sea que se obtenga la certificación o se completen los requisitos enumerados anteriormente, cada joven que aprenda primeros auxilios en este nivel debe saber dónde se guarda el botiquín de primeros auxilios del club, la escuela y/o la iglesia y cómo utilizarlo. Todos los botiquines de primeros auxilios deben incluir guantes y protección para los ojos junto con los suministros regulares.
References