Difference between revisions of "AY Honors/First Aid, Standard/Answer Key"
m |
|||
| (39 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
| − | {{ | + | {{HonorSubpage}} |
| − | + | <section begin="Body" /> | |
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=Prologue|dispreq= }} | ||
| + | {{CloseReq}} <!-- Prologue --> | ||
| − | + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=1}} | |
| + | <noinclude><translate><!--T:56--> | ||
| + | </noinclude> | ||
| + | <!-- 1. Know the basic principles for mouth-to-mouth breathing and the treatment for an obstructed airway. --> | ||
| + | {{:AY Honors/First aid/Rescue_breathing}} | ||
| − | + | <!--T:57--> | |
| − | + | <noinclude></translate></noinclude> | |
| − | {{: | + | {{CloseReq}} <!-- 1 --> |
| − | + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=2}} | |
| − | + | <noinclude><translate></noinclude> | |
| − | ===Heart Attack=== | + | <!-- 2. What is the difference between a heart attack and a stroke and the treatment for each? --> |
| − | {{: | + | ===Heart Attack=== <!--T:58--> |
| + | {{:AY Honors/First aid/Heart_attack}} | ||
===Stroke=== | ===Stroke=== | ||
| − | {{: | + | {{:AY Honors/First aid/Stroke}} |
| − | ==3. Know the proper procedure for assisting a bleeding victim. | + | <!--T:59--> |
| − | {{: | + | <noinclude></translate></noinclude> |
| − | ==4. Know the pressure points and how to correctly apply pressure at those points. | + | {{CloseReq}} <!-- 2 --> |
| − | {{: | + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=3}} |
| − | ==5. Know the proper method of applying a tourniquet and when to apply one. | + | <noinclude><translate><!--T:60--> |
| − | A '''tourniquet''' is a tightly tied band applied around a body part (an arm or a leg) sometimes used in an attempt to stop severe traumatic bleeding. Severe bleeding means the loss of more than 1,000 ml (1 litre) of blood. | + | </noinclude> |
| + | <!-- 3. Know the proper procedure for assisting a bleeding victim. --> | ||
| + | {{:AY Honors/First aid/Bleeding}} | ||
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 3 --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=4}} | ||
| + | <noinclude><translate><!--T:61--> | ||
| + | </noinclude> | ||
| + | <!-- 4. Know the pressure points and how to correctly apply pressure at those points. --> | ||
| + | {{:AY Honors/First aid/Pressure_points}} | ||
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 4 --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=5}} | ||
| + | <noinclude><translate><!--T:62--> | ||
| + | </noinclude> | ||
| + | <!-- 5. Know the proper method of applying a tourniquet and when to apply one. --> | ||
| + | A '''tourniquet''' is a tightly tied band applied around a body part (an arm or a leg) sometimes used in an attempt to stop severe traumatic bleeding. Severe bleeding means the loss of more than 1,000 ml (1 litre) of blood. This flow of blood can soak a paper or cloth handkerchief in a few seconds. In such a situation, the bleeding will cause the death of the casualty in seconds to minutes. | ||
| + | <!--T:8--> | ||
A tourniquet is a ''last resort'' method of bleeding control. Other methods that should be applied first and in conjunction, if possible, include: | A tourniquet is a ''last resort'' method of bleeding control. Other methods that should be applied first and in conjunction, if possible, include: | ||
| + | <!--T:9--> | ||
* direct pressure | * direct pressure | ||
* elevation of the limb or wound above the heart | * elevation of the limb or wound above the heart | ||
| Line 28: | Line 53: | ||
* blood-clotting agents or bandages | * blood-clotting agents or bandages | ||
| − | Even in cases of amputation, most bleeding can be controlled through these alternative methods. | + | <!--T:10--> |
| + | Even in cases of amputation, most bleeding can be controlled through these alternative methods. The rare exception is when a limb is shattered by massive trauma or when a major blood vessel is torn along its length. Even in these cases, the use of a pressure point above the wound is strongly preferred. | ||
| − | As the tourniquet stops blood flow to the limb, it can cause the death of the limb, forcing the later surgical amputation of the limb just below the level the tourniquet is applied. | + | <!--T:11--> |
| + | As the tourniquet stops blood flow to the limb, it can cause the death of the limb, forcing the later surgical amputation of the limb just below the level the tourniquet is applied. This is likely to occur when the tourniquet stays in place several hours. In any event, once a tourniquet has been applied, advanced medical care from a doctor or hospital ''will'' be required to salvage the limb if not save the life of the patient. | ||
| − | The decision to employ a tourniquet should be made by an emergency medical technician or preferably a doctor if at all possible. | + | <!--T:12--> |
| + | The decision to employ a tourniquet should be made by an emergency medical technician or preferably a doctor if at all possible. But when severe external bleeding cannot be controlled by other means, a tourniquet may be the only way for a first-aider to save the casualty. | ||
| + | <!--T:13--> | ||
Most civilian first aid instruction in the United States no longer teaches the use of the tourniquet for the following reasons: | Most civilian first aid instruction in the United States no longer teaches the use of the tourniquet for the following reasons: | ||
* the effectiveness of direct pressure, elevation and pressure points (controlling severe bleeding in up to 90% of cases as estimated by US medical sources) | * the effectiveness of direct pressure, elevation and pressure points (controlling severe bleeding in up to 90% of cases as estimated by US medical sources) | ||
| Line 41: | Line 70: | ||
* the rare nature of injuries that require tourniquets, which typically occur in unusual settings such as working with agricultural or industrial machinery and the battlefield | * the rare nature of injuries that require tourniquets, which typically occur in unusual settings such as working with agricultural or industrial machinery and the battlefield | ||
| + | <!--T:14--> | ||
The use of a tourniquet by a layperson in countries where it is considered outside the scope of practice of first aid may result in civil lawsuits and/or criminal charges, especially if the application was later found to have been unnecessary. | The use of a tourniquet by a layperson in countries where it is considered outside the scope of practice of first aid may result in civil lawsuits and/or criminal charges, especially if the application was later found to have been unnecessary. | ||
| − | ==6. Know the causes of shock and demonstrate its proper treatment. | + | <!--T:63--> |
| − | {{: | + | <noinclude></translate></noinclude> |
| − | ==7. Know the proper procedure for assisting a victim of poisoning. | + | {{CloseReq}} <!-- 5 --> |
| − | {{: | + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=6}} |
| − | ==8. Know the proper procedure for assisting a burn victim. | + | <noinclude><translate><!--T:64--> |
| − | ===Thermal Burns=== | + | </noinclude> |
| − | {{:First aid/Burns}} | + | <!-- 6. Know the causes of shock and demonstrate its proper treatment. --> |
| + | {{:AY Honors/First aid/Shock}} | ||
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 6 --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=7}} | ||
| + | <noinclude><translate><!--T:65--> | ||
| + | </noinclude> | ||
| + | <!-- 7. Know the proper procedure for assisting a victim of poisoning. --> | ||
| + | {{:AY Honors/First aid/Poison}} | ||
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 7 --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=8}} | ||
| + | <noinclude><translate></noinclude> | ||
| + | <!-- 8. Know the proper procedure for assisting a burn victim. --> | ||
| + | ===Thermal Burns=== <!--T:66--> | ||
| + | {{:AY Honors/First aid/Burns}} | ||
===Chemical Burns=== | ===Chemical Burns=== | ||
| − | {{: | + | {{:AY Honors/First aid/Chemical_burn}} |
| − | ==9. Know how to properly apply the following bandages:== | + | <!--T:67--> |
| − | + | <noinclude></translate></noinclude> | |
| − | Start by laying a strip of roller bandage along the length of the limb, from the larger portion to the smaller (for example, from the elbow to the wrist, or from the knee to the ankle). | + | {{CloseReq}} <!-- 8 --> |
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=9}} | ||
| + | <noinclude><translate><!--T:68--> | ||
| + | </noinclude> | ||
| + | <!-- 9. Know how to properly apply the following bandages: --> | ||
| + | <noinclude></translate></noinclude> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=9a}} | ||
| + | <noinclude><translate><!--T:69--> | ||
| + | Start by laying a strip of roller bandage along the length of the limb, from the larger portion to the smaller (for example, from the elbow to the wrist, or from the knee to the ankle). Then make two or three turns around the smaller part of the limb, and then wind upward in a spiral fashion, covering the first part of the bandage that was laid down. For an open spiral, leave gaps between successive windings. This is useful for holding dressings in place over a large area, as needed in the case of a burn. For a closed spiral, overlap each winding. Secure at the top by tying the two ends of the bandage together with a square knot. | ||
| + | {{:AY Honors/Knot/Square}} | ||
| − | == | + | <!--T:70--> |
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 9a --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=9b}} <!--T:17--> | ||
| + | <noinclude><translate><!--T:71--> | ||
| + | </noinclude> | ||
| − | {{: | + | <!--T:18--> |
| + | {{:AY Honors/First aid/Ankle_splint}} | ||
| + | <!--T:19--> | ||
The figure-eight bandage can also be used on the hand, wrist, elbow, and knee. | The figure-eight bandage can also be used on the hand, wrist, elbow, and knee. | ||
| − | == | + | <!--T:72--> |
| − | Begin by laying the bandage along the length of the injured finger, leaving the end extending a couple of inches to the center of the palm. | + | <noinclude></translate></noinclude> |
| + | {{CloseReq}} <!-- 9b --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=9c}} <!--T:20--> | ||
| + | <noinclude><translate><!--T:73--> | ||
| + | </noinclude> | ||
| + | Begin by laying the bandage along the length of the injured finger, leaving the end extending a couple of inches to the center of the palm. Then take the bandage over the fingertip, and going back down again on the other side to the base of the finger. Twist the bandage, and begin spiraling towards the fingertip. When the top joint of the finger is reached, spiral downwards again towards the base of the finger. Tie the two ends together with a square knot to secure the bandage. | ||
| − | == | + | <!--T:74--> |
| − | {{: | + | <noinclude></translate></noinclude> |
| + | {{CloseReq}} <!-- 9c --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=9d}} <!--T:21--> | ||
| + | <noinclude><translate><!--T:75--> | ||
| + | </noinclude> | ||
| + | {{:AY Honors/First aid/Cravat_bandage_to_head}} | ||
| − | ==10. Know how to apply the following splints:== | + | <!--T:76--> |
| − | + | <noinclude></translate></noinclude> | |
| − | {{: | + | {{CloseReq}} <!-- 9d --> |
| − | == | + | {{CloseReq}} <!-- 9 --> |
| − | {{: | + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=10}} |
| − | == | + | <noinclude><translate><!--T:77--> |
| − | {{: | + | </noinclude> |
| − | == | + | <!-- 10. Know how to apply the following splints: --> |
| − | {{: | + | <noinclude></translate></noinclude> |
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=10a}} | ||
| + | <noinclude><translate><!--T:78--> | ||
| + | </noinclude> | ||
| + | {{:AY Honors/First aid/Upper_arm_splint}} | ||
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 10a --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=10b}} | ||
| + | <noinclude><translate><!--T:79--> | ||
| + | </noinclude> | ||
| + | {{:AY Honors/First aid/Forearm_splint}} | ||
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 10b --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=10c}} | ||
| + | <noinclude><translate><!--T:80--> | ||
| + | </noinclude> | ||
| + | {{:AY Honors/First aid/Ankle_splint}} | ||
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 10c --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=10d}} | ||
| + | <noinclude><translate><!--T:81--> | ||
| + | </noinclude> | ||
| + | {{:AY Honors/First_aid/Kneecap_splint}} | ||
| − | ==11. Know the proper treatment for the following:== | + | <!--T:82--> |
| − | + | <noinclude></translate></noinclude> | |
| − | {{: | + | {{CloseReq}} <!-- 10d --> |
| + | {{CloseReq}} <!-- 10 --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=11}} | ||
| + | <noinclude><translate><!--T:83--> | ||
| + | </noinclude> | ||
| + | <!-- 11. Know the proper treatment for the following: --> | ||
| + | <noinclude></translate></noinclude> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=11a}} | ||
| + | <noinclude><translate><!--T:84--> | ||
| + | </noinclude> | ||
| + | {{:AY Honors/First aid/Head_injury}} | ||
| − | == | + | <!--T:85--> |
| − | {{: | + | <noinclude></translate></noinclude> |
| + | {{CloseReq}} <!-- 11a --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=11b}} <!--T:24--> | ||
| + | <noinclude><translate><!--T:86--> | ||
| + | </noinclude> | ||
| + | {{:AY Honors/First aid/Internal injuries}} | ||
| − | == | + | <!--T:87--> |
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 11b --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=11c}} <!--T:25--> | ||
| + | <noinclude><translate><!--T:88--> | ||
| + | </noinclude> | ||
A gunshot wound is a medical emergency and will require treatment at a medical facility. | A gunshot wound is a medical emergency and will require treatment at a medical facility. | ||
| − | First, control any bleeding by using the pressure points and by elevating the injured area. | + | First, control any bleeding by using the pressure points and by elevating the injured area. Do not try to remove the bullet, it may help a doctor to determine the extent of the injury, and its removal may increase the bleeding. Cut or tear away any clothing covering the wound. Do not pour any liquids into the wound. Wipe any debris away from the wound, but be careful not to wipe it towards the wound - always wipe ''away'' from the wound. Cover the wound with a bandage and fasten it securely so that it will not hang on anything during transport or slip off. Reassure the victim and get him to a hospital as soon as possible. |
| − | == | + | <!--T:89--> |
| − | Wounds that involve the eyelids or the soft tissue around the eye must be handled carefully to | + | <noinclude></translate></noinclude> |
| + | {{CloseReq}} <!-- 11c --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=11d}} <!--T:26--> | ||
| + | <noinclude><translate><!--T:90--> | ||
| + | </noinclude> | ||
| + | Wounds that involve the eyelids or the soft tissue around the eye must be handled carefully to avoid further damage. If the injury does not involve the eyeball, apply a sterile compress and hold it in place with a firm bandage. If the eyeball appears to be injured, use a loose bandage. (Remember that you must NEVER attempt to remove any object that is embedded in the eyeball or that has penetrated it; just apply a dry, sterile compress to cover both eyes, and hold the compress in place with a loose bandage). Any person who has suffered a facial wound that involves the eye, the eyelids, or the tissues around the eye must receive medical attention as soon as possible. Be sure to keep the victim lying down. Use a stretcher for transport. | ||
| − | Many eye wounds contain foreign objects. | + | <!--T:27--> |
| + | Many eye wounds contain foreign objects. Dirt, coal, cinders, eyelashes, bits of metal, and a variety of other objects may become lodged in the eye. Since even a small piece of dirt is intensely irritating to the eye, the removal of such objects is important. However, the eye is easily damaged. Impairment of vision (or even total loss of vision) can result from fumbling, inexpert attempts to remove foreign objects from the eye. The following precautions must be observed: | ||
* '''DO NOT''' allow the victim to rub the eye. | * '''DO NOT''' allow the victim to rub the eye. | ||
| − | * '''DO NOT''' press against the eye or manipulate it in any way that might cause the object to become embedded in the tissues of the eye. | + | * '''DO NOT''' press against the eye or manipulate it in any way that might cause the object to become embedded in the tissues of the eye. Be very gentle; roughness is almost sure to cause injury to the eye. |
* '''DO NOT''' use such things as knives, toothpicks, matchsticks, or wires to remove the object. | * '''DO NOT''' use such things as knives, toothpicks, matchsticks, or wires to remove the object. | ||
| − | * '''DO NOT UNDER ANY CIRCUMSTANCES ATTEMPT | + | * '''DO NOT UNDER ANY CIRCUMSTANCES ATTEMPT TO REMOVE AN OBJECT THAT IS EMBEDDED IN THE EYEBALL OR THAT HAS PENETRATED THE EYE!''' If you see a splinter or other object sticking out from the eyeball, leave it alone! Only specially trained medical personnel can hope to save the victim’s sight if an object has actually penetrated the eyeball. |
| + | <!--T:28--> | ||
Small objects that are lodged on the surface of the eye or on the membrane lining the eyelids can usually be removed by the following procedures: | Small objects that are lodged on the surface of the eye or on the membrane lining the eyelids can usually be removed by the following procedures: | ||
| − | # Try | + | # Try to wash the eye gently with lukewarm, sterile water. A sterile medicine dropper or a sterile syringe can be used for this purpose. Have the victim lie down, with the head turned slightly to one side. Hold the eyelids apart. Direct the flow of water to the inside corner of the eye, and let it run down to the outside corner. Do not let the water fall directly onto the eyeball. |
| − | # Gently pull the lower lid down, and instruct the victim to look up. If you can see the object, try to remove it with the corner of a clean handkerchief or with a small moist cotton swab. You can make the swab by twisting cotton around a wooden applicator, not too tightly, and moistening it with sterile water. <br>'''CAUTION:''' Never use dry cotton anywhere near the eye. | + | # Gently pull the lower lid down, and instruct the victim to look up. If you can see the object, try to remove it with the corner of a clean handkerchief or with a small moist cotton swab. You can make the swab by twisting cotton around a wooden applicator, not too tightly, and moistening it with sterile water. <br>'''CAUTION:''' Never use dry cotton anywhere near the eye. It will stick to the eyeball or to the inside of the lids, and you will have the problem of removing it as well as the original object. |
| − | # If you cannot see the object when the lower lid is pulled | + | # If you cannot see the object when the lower lid is pulled down, turn the upper lid back over a smooth wooden applicator. Tell the victim to look down. Place the applicator lengthwise across the center of the upper lid. Grasp the lashes of the upper lid gently but firmly. Press gently with the applicator. Pull up on the eyelashes, turning the lid back over the applicator. If you can see the object, try to remove it with a moist cotton swab or with the corner of a clean handkerchief. |
| − | # If the foreign object cannot be removed by any of the above methods, | + | # If the foreign object cannot be removed by any of the above methods, '''DO NOT MAKE ANY FURTHER ATTEMPTS TO REMOVE IT.''' Instead, place a small, thick gauze dressing over both eyes and hold it in place with a loose bandage. This limits movement of the injured eye. |
# Get medical help for the victim at the earliest opportunity. | # Get medical help for the victim at the earliest opportunity. | ||
| − | == | + | <!--T:91--> |
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 11d --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=11e}} <!--T:29--> | ||
| + | <noinclude><translate><!--T:92--> | ||
| + | </noinclude> | ||
'''Animal Bites''' | '''Animal Bites''' | ||
| − | {{: | + | <!--T:30--> |
| + | {{:AY Honors/First aid/Animal bites}} | ||
| + | <!--T:31--> | ||
'''Insect Bites''' | '''Insect Bites''' | ||
| − | {{: | + | <!--T:32--> |
| + | {{:AY Honors/First aid/Insect bites}} | ||
| − | == | + | <!--T:93--> |
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 11e --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=11f}} <!--T:33--> | ||
| + | <noinclude><translate><!--T:94--> | ||
| + | </noinclude> | ||
'''Fainting''' | '''Fainting''' | ||
| − | {{: | + | <!--T:34--> |
| + | {{:AY Honors/First aid/Fainting}} | ||
| + | <!--T:35--> | ||
'''Epilepsy''' | '''Epilepsy''' | ||
| − | {{: | + | <!--T:36--> |
| + | {{:AY Honors/First aid/Epilepsy}} | ||
| − | == | + | <!--T:95--> |
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 11f --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=11g}} <!--T:37--> | ||
| + | <noinclude><translate><!--T:96--> | ||
| + | </noinclude> | ||
'''Heat Exhaustion''' | '''Heat Exhaustion''' | ||
| − | {{: | + | <!--T:38--> |
| + | {{:AY Honors/First aid/Heat exhaustion}} | ||
| + | <!--T:39--> | ||
'''Heat Stroke''' | '''Heat Stroke''' | ||
| − | {{: | + | <!--T:40--> |
| + | {{:AY Honors/First aid/Heat stroke}} | ||
| + | <!--T:41--> | ||
'''Hypothermia''' | '''Hypothermia''' | ||
| − | {{: | + | <!--T:42--> |
| + | {{:AY Honors/First aid/Hypothermia}} | ||
| + | <!--T:43--> | ||
'''Frostbite''' | '''Frostbite''' | ||
| − | {{: | + | <!--T:44--> |
| − | + | {{:AY Honors/First aid/Frostbite}} | |
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | == | + | <!--T:97--> |
| − | {{: | + | <noinclude></translate></noinclude> |
| + | {{CloseReq}} <!-- 11g --> | ||
| + | {{CloseReq}} <!-- 11 --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=12}} | ||
| + | <noinclude><translate><!--T:98--> | ||
| + | </noinclude> | ||
| + | <!-- 12. Know what to do in an electrical emergency. --> | ||
| + | {{:AY Honors/First aid/Electric wire contact}} | ||
| − | == | + | <!--T:99--> |
| − | {{: | + | <noinclude></translate></noinclude> |
| + | {{CloseReq}} <!-- 12 --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=13}} | ||
| + | <noinclude><translate><!--T:100--> | ||
| + | </noinclude> | ||
| + | <!-- 13. Know how to escape from a fire. --> | ||
| + | {{:AY Honors/First aid/Smoke fire}} | ||
| − | == | + | <!--T:101--> |
| − | With the advent of the cell phone, the most effective way of obtaining help in an emergency is by calling 911. | + | <noinclude></translate></noinclude> |
| + | {{CloseReq}} <!-- 13 --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=14}} | ||
| + | <noinclude><translate><!--T:102--> | ||
| + | </noinclude> | ||
| + | <!-- 14. Know how to obtain help in an emergency --> | ||
| + | With the advent of the cell phone, the most effective way of obtaining help in an emergency is by calling 911. Most cell phones are equipped with a GPS module which allows their location to be pin-pointed by a satellite. The cell phone automatically relays this information to the 911 operator. | ||
| − | However, sometimes a cell phone is either not available, or it is not within range of a cell phone antenna tower. | + | <!--T:49--> |
| + | However, sometimes a cell phone is either not available, or it is not within range of a cell phone antenna tower. If you find yourself facing an emergency in the wilderness, you may have to attempt to signal aircraft. Three ways of doing that are presented here: | ||
| − | {{: | + | <!--T:50--> |
| + | {{:AY Honors/First aid/Signaling aircraft}} | ||
| − | == | + | <!--T:103--> |
| − | + | <noinclude></translate></noinclude> | |
| − | {{: | + | {{CloseReq}} <!-- 14 --> |
| − | == | + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=15}} |
| − | {{: | + | <noinclude><translate><!--T:104--> |
| − | == | + | </noinclude> |
| − | {{: | + | <!-- 15. Know the following rescue carries: --> |
| − | == | + | <noinclude></translate></noinclude> |
| − | {{: | + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=15a}} |
| − | == | + | <noinclude><translate><!--T:105--> |
| − | {{: | + | </noinclude> |
| + | {{:AY Honors/First aid/Shoulder drag}} | ||
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 15a --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=15b}} | ||
| + | <noinclude><translate><!--T:106--> | ||
| + | </noinclude> | ||
| + | {{:AY Honors/First aid/Blanket drag}} | ||
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 15b --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=15c}} | ||
| + | <noinclude><translate><!--T:107--> | ||
| + | </noinclude> | ||
| + | {{:AY Honors/First aid/Two person carry}} | ||
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 15c --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=15d}} | ||
| + | <noinclude><translate><!--T:108--> | ||
| + | </noinclude> | ||
| + | {{:AY Honors/First aid/Carry by extremities}} | ||
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 15d --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=15e}} | ||
| + | <noinclude><translate><!--T:109--> | ||
| + | </noinclude> | ||
| + | {{:AY Honors/First aid/Improvised litter}} | ||
| − | == | + | <!--T:110--> |
| − | {{: | + | <noinclude></translate></noinclude> |
| − | == | + | {{CloseReq}} <!-- 15e --> |
| − | {{: | + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=15f}} <!--T:52--> |
| + | <noinclude><translate><!--T:111--> | ||
| + | </noinclude> | ||
| + | {{:AY Honors/First aid/Hammock carry}} | ||
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 15f --> | ||
| + | {{ansreq|page={{#titleparts:{{PAGENAME}}|2|1}}|num=15g}} | ||
| + | <noinclude><translate><!--T:112--> | ||
| + | </noinclude> | ||
| + | {{:AY Honors/First aid/Litter carry}} | ||
| − | ==References== | + | <!--T:113--> |
| + | <noinclude></translate></noinclude> | ||
| + | {{CloseReq}} <!-- 15g --> | ||
| + | {{CloseReq}} <!-- 15 --> | ||
| + | <noinclude><translate></noinclude> | ||
| + | ==References== <!--T:53--> | ||
*http://www.tpub.com/content/medical/10669-c/index.htm | *http://www.tpub.com/content/medical/10669-c/index.htm | ||
*http://www.tpub.com/content/medical/14295/index.htm | *http://www.tpub.com/content/medical/14295/index.htm | ||
*http://www.tpub.com/content/aviationandaccessories/TM-1-1680-359-10/index.htm TM-1-1680-359-10 | *http://www.tpub.com/content/aviationandaccessories/TM-1-1680-359-10/index.htm TM-1-1680-359-10 | ||
*http://www.cert-la.com/liftcarry/Liftcarry.htm | *http://www.cert-la.com/liftcarry/Liftcarry.htm | ||
| + | <noinclude></translate></noinclude> | ||
| − | [[Category: | + | [[Category:Instructor Required{{GetLangSuffix}}|{{SUBPAGENAME}}]] |
| + | {{CloseHonorPage}} | ||
Latest revision as of 21:17, 1 January 2023
If residing in the United States or another country in which Red Cross instruction is given, satisfactorily pass the Red Cross Examination in Standard First Aid and receive your certificate.
In British countries pass the examination in St. John Ambulance and receive certificate for the same.
Or complete the following requirements:
1
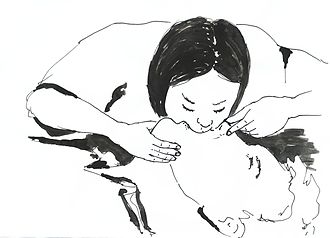
- If the patient is breathing, do not administer rescue breathing. Rescue breathing is an emergency treatment that may help the victim regain the ability to breathe on his own.
- Tilt the victim's head back, and lift their chin (head-tilt chin-lift). The head will not remain in this position by itself, you must maintain the head-tilt chin-lift throughout.
- In certain cases, you may not be able to give rescue breaths through the mouth - blow into the nose and seal the mouth instead.
- Pinch the victim's nose
- Put your mouth on the mouth of the victim, maintaining a good seal, and blow into the mouth. These breaths should be gentle and last no longer than 2 seconds to prevent air from entering the stomach.
When you have given two rescue breaths, begin chest compressions if you are trained to do so. Otherwise, continue with rescue breathing: 2 breaths every 5 seconds.
If the victim has recovered spontaneous respiration, put him in the recovery position, cover him, and monitor his breathing on a regular basis until an ambulance arrives.
2
Heart Attack
A heart attack is when blood supply to part of the heart is interrupted causing heart tissue to die. Symptoms of a heart attack include severe chest pain, looking pale, sweating, and feeling sick. A heart attack is a medical emergency, and it is a leading cause of death for both men and women.
First aid includes the following:
- Seek emergency medical assistance immediately.
- Help the patient to rest in a position which minimizes breathing difficulties. A half-sitting position with knees bent is often recommended.
- Give access to more oxygen, e.g. by opening the window and widening the collar for easier breathing; but keep the patient warm, e.g. by a blanket or a jacket
- Give aspirin, if the patient is not allergic to aspirin. Aspirin inhibits formation of further blood clots.
- Non-coated or soluble preparations are preferred. These should be chewed or dissolved, respectively, to facilitate quicker absorption. If the patient cannot swallow, the aspirin can be placed under the tongue.
- U.S. guidelines recommend a dose of 160 – 325 mg.
- Australian guidelines recommend a dose of 150 – 300 mg.
- If it has been prescribed for the patient, give nitroglycerin tablets under the tongue.
- Monitor pulse, breathing, level of consciousness and, if possible, the blood pressure of the patient continually.
- Administer CPR if the victim is unconscious and non-breathing.
Stroke
A stroke is caused by an interruption of the arterial blood supply to a portion of the brain. This interruption may be caused by hardening of the arteries or by a clot forming in the brain. Tissue damage and loss of function result. Onset of a stroke is sudden, with little or no warning. The first signs include weakness or paralysis, especially on one side of the body. Muscles of the face may be particularly affected. The victim’s level of consciousness varies from alert to unresponsive. Difficulty speaking or understanding language; dizziness; sudden, severe headache; distorted, dim or patchy vision are all symptoms of stroke.
If the victim has sudden onset of any 2 or more of these signs and symptoms, call an ambulance immediately. First aid for a stroke is mainly supportive. Special attention must be paid to the victim’s airway, since he may not be able to keep it clear.
- Call an ambulance
- Place the victim in on their side, with the affected side down
- Act in a calm, reassuring manner, and keep any onlookers quiet since the victim may be able to hear what is going on.
- Carefully monitor the victim’s vital signs and keep a log. Pay special attention to respirations, and pulse strength and rate (take the pulse in the neck).
3
If you see a person who is bleeding heavily, you can do the following:
- Press hard onto the wound to stop the bleeding.
- If an arm or leg is cut, elevate the limb.
- Cover with a clean pad and apply a bandage.
- Check that the bleeding has stopped. If it has not, add another pad, and bandage, do not remove previous bandage.
- If you have bandaged a limb, check frequently that the fingers and toes remain warm. If fingers and toes are getting cold, loosen the bandage to let the blood circulate.
- For severe bleeding (5 cups of blood or more), get the person to a hospital for stitches (and possibly immunization against Tetanus) keeping the limb raised.
4
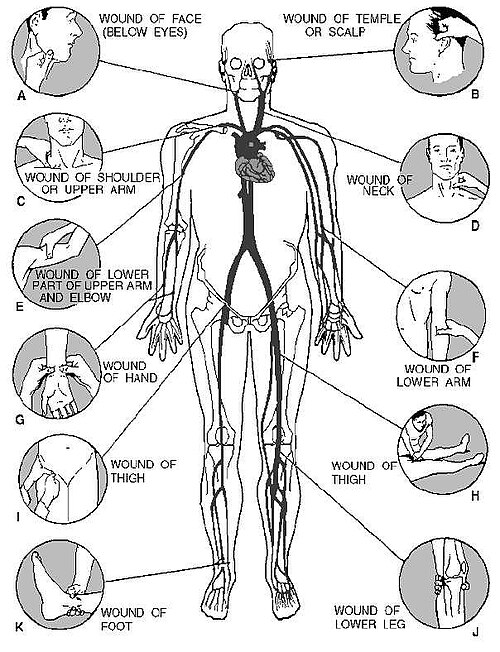
The usual way to control bleeding is to put pressure directly onto the wound, either with the hand directly or with a dressing of some sort (bandage, handkerchief, tea towel etc.). Do not forget that any wound which is not controlled within a minute or two is a medical emergency; and any deep or large wound must receive medical attention as soon as possible.
It is sometimes not possible to press directly on a wound: for example, there may be a foreign object inside the wound, or a broken bone protruding outside, or the wound may be too large or be inaccessible (e.g. if the limb is trapped by some immovable object). In this case, the only way to control the bleeding is to compress blood vessels over particular pressure points (usually where arteries cross over bones near to the surface of the skin). This technique can be used to control external bleeding from arm wounds and leg wounds.
The correct point is determined by finding a pulse on a victim similar to that felt in the wrist when taking one's own pulse. This point could be located in the wrist, the arm (on the soft underside of the elbow), the groin, or behind the knee. This is the position where a rhythmical pulsation can be felt. Pressure can then be applied over this point -- the artery -- to control bleeding.
Once an artery is compressed over a pressure point, it must not be compressed for more than 10 minutes: any longer in one go can cause irreversible damage to the limb. Typically pressure would be applied for 10 minutes, then released for a couple, then reapplied and so on.
5
A tourniquet is a tightly tied band applied around a body part (an arm or a leg) sometimes used in an attempt to stop severe traumatic bleeding. Severe bleeding means the loss of more than 1,000 ml (1 litre) of blood. This flow of blood can soak a paper or cloth handkerchief in a few seconds. In such a situation, the bleeding will cause the death of the casualty in seconds to minutes.
A tourniquet is a last resort method of bleeding control. Other methods that should be applied first and in conjunction, if possible, include:
- direct pressure
- elevation of the limb or wound above the heart
- the use of a pressure point to slow the artery above the injury(s)
- blood-clotting agents or bandages
Even in cases of amputation, most bleeding can be controlled through these alternative methods. The rare exception is when a limb is shattered by massive trauma or when a major blood vessel is torn along its length. Even in these cases, the use of a pressure point above the wound is strongly preferred.
As the tourniquet stops blood flow to the limb, it can cause the death of the limb, forcing the later surgical amputation of the limb just below the level the tourniquet is applied. This is likely to occur when the tourniquet stays in place several hours. In any event, once a tourniquet has been applied, advanced medical care from a doctor or hospital will be required to salvage the limb if not save the life of the patient.
The decision to employ a tourniquet should be made by an emergency medical technician or preferably a doctor if at all possible. But when severe external bleeding cannot be controlled by other means, a tourniquet may be the only way for a first-aider to save the casualty.
Most civilian first aid instruction in the United States no longer teaches the use of the tourniquet for the following reasons:
- the effectiveness of direct pressure, elevation and pressure points (controlling severe bleeding in up to 90% of cases as estimated by US medical sources)
- the increased difficulty of reattaching an amputated limb when a tourniquet has been applied to the victim
- unnecessary use by poorly trained bystanders
- the unavoidable risks to both limb and life even when properly employed
- the rare nature of injuries that require tourniquets, which typically occur in unusual settings such as working with agricultural or industrial machinery and the battlefield
The use of a tourniquet by a layperson in countries where it is considered outside the scope of practice of first aid may result in civil lawsuits and/or criminal charges, especially if the application was later found to have been unnecessary.
6
Shock is a medical condition where the delivery of oxygen and nutrients is insufficient to meet the body's needs. The main carrier of oxygen and nutrients in the body is the blood, so anytime there is a loss of blood, there is a risk of shock. Shock is a life-threatening emergency.
First aid treatment of shock includes:
- Immediate reassurance and comforting the victim if conscious.
- If alone, go for help. If not, send someone to go for help and someone stay with the victim.
- Ensure that the airway is clear and check for breathing. Place the victim in the recovery position if possible.
- Attempt to stop any obvious bleeding.
- Cover the victim with a blanket or jacket, but not too thick or it may cause a dangerous drop in blood pressure.
- Do not give a drink. Moisten lips if requested.
- Prepare for cardiopulmonary resuscitation (CPR).
- Give as much information as possible when the ambulance arrives.
7
With poison container in hand, call the local poison control center and do NOT try to make the patient vomit. Only induce vomiting if a poison center worker or a doctor advises you to do so. If the poison is on the skin or clothes, remove the clothing and wash with a large amount of water. If poison gets in the eyes, flush the eyes with clean water for 10 minutes.
Get the victim to a hospital as soon as possible, and if possible, bring the poison container with you.
8
Thermal Burns
Burns should be immediately immersed in cold running water, or shower for large area. Do not wait to remove clothes. This should be maintained for at least 10-15 minutes.
Continue for at least 1 hour with cold pack, partially insulated with clean fabric (cotton, thin toweling), or further immersion in iced water. Blistered or open burn wounds should be cleaned and covered with non-adhesive gauze (preferably bactericidal) and cotton dressing. DO NOT use butter, oils or any similar treatment which can trap heat and increase risk of infection. Also do not use antiseptics that may aggravate sensitive skin.
Consult a medical physician immediately for any large, deep, infected or otherwise serious burn.
Aloe vera extract, silverdene (Silver sulfadiazine), topical analgaesics and NSAID are commonly used medications. Consult a doctor before use.
Burns are sustained by electricity, heat , chemical or radiation (sunburn). There are three levels of burns, including first degree burns (Superficial burn), second degree burns (Partial thickness burn) and third degree burns (Full thickness burn). The first degree burn is typical sunburn with symptoms such as redness of the skin and pain. Second degree often has blisters and severe pain. Third degree can be caused by fires and caustic chemicals. Often the victim will feel no pain because the nerves have been destroyed, even though the skin is deeply charred.
Burns that cover more than ten percent of the body, or are larger than the casualty's palm, are medical emergencies and need to be treated as such. Also ANY burns to the face, hands or groin should be considered critical and require an examination by a physician.
Chemical Burns
1. For wet chemicals, immediately flush the area with large amounts of water, using a shower or hose, if available. Do not apply water too forcefully. Continue to flood the area while the clothing, including shoes and socks, is being removed. Continue to flush with running water for at least 20 minutes.
- For dry chemicals, brush off the chemical, then flush with water as above.
- For acid burns caused by phenol (carbolic acid), wash the affected area with alcohol because phenol is not water soluble; then wash with water. If alcohol is not available, flushing with water is better than no treatment at all.
2. Call an ambulance
9
9a
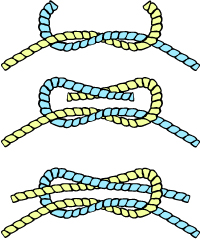
Start by laying a strip of roller bandage along the length of the limb, from the larger portion to the smaller (for example, from the elbow to the wrist, or from the knee to the ankle). Then make two or three turns around the smaller part of the limb, and then wind upward in a spiral fashion, covering the first part of the bandage that was laid down. For an open spiral, leave gaps between successive windings. This is useful for holding dressings in place over a large area, as needed in the case of a burn. For a closed spiral, overlap each winding. Secure at the top by tying the two ends of the bandage together with a square knot.
| Square Knot |
|---|
|
Use: Also known as a Reef knot, the Square Knot is easily learned and useful for many situations. It is most commonly used to tie two lines together at the ends. This knot is used at sea in reefing and furling sails. It is used in first aid to tie off a bandage or a sling because the knot lies flat.
How to tie:
WARNING: Do not rely on this knot to hold weight in a life or death situation. It has been known to fail.
|
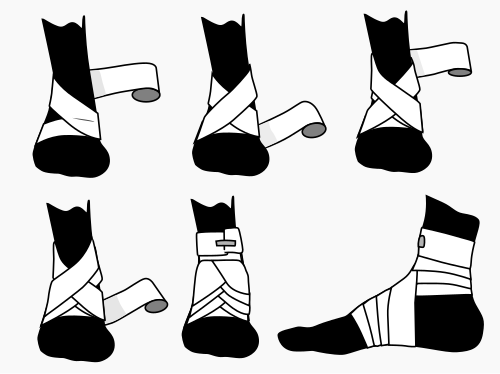
9b
The figure-eight bandage is used for dressings of the ankle, as well as for supporting a sprain. While keeping the foot at a right angle, start a 3-inch bandage around the instep for several turns to anchor it. Carry the bandage upward over the instep and around behind the ankle, forward, and again across the instep and down under the arch, thus completing one figure-eight. Continue the figure-eight turns, overlapping one-third to one-half the width of the bandage and with an occasional turn around the ankle, until the compress is secured or until adequate support is obtained.
The figure-eight bandage can also be used on the hand, wrist, elbow, and knee.
9c
Begin by laying the bandage along the length of the injured finger, leaving the end extending a couple of inches to the center of the palm. Then take the bandage over the fingertip, and going back down again on the other side to the base of the finger. Twist the bandage, and begin spiraling towards the fingertip. When the top joint of the finger is reached, spiral downwards again towards the base of the finger. Tie the two ends together with a square knot to secure the bandage.
9d
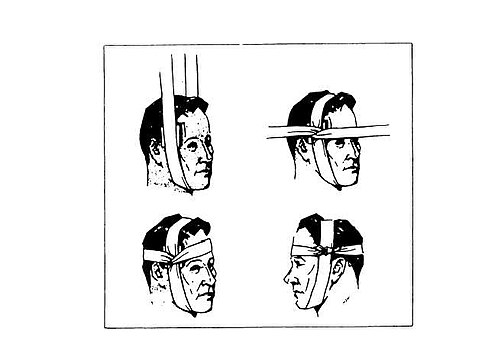
This bandage is useful to control bleeding from wounds of the scalp or forehead. After placing a compress over the wound, place the center of the cravat over the compress and carry the ends around to the opposite side; cross them, continue to carry them around to the starting point, and tie in a square knot.
| Square Knot |
|---|
|
Use: Also known as a Reef knot, the Square Knot is easily learned and useful for many situations. It is most commonly used to tie two lines together at the ends. This knot is used at sea in reefing and furling sails. It is used in first aid to tie off a bandage or a sling because the knot lies flat.
How to tie:
WARNING: Do not rely on this knot to hold weight in a life or death situation. It has been known to fail.
|
10
10a
The signs of fracture of the upper arm include pain, tenderness, swelling, and a wobbly motion at the point of fracture. If the fracture is near the elbow, the arm is likely to be straight with no bend at the elbow. If the fracture is open, stop the bleeding and treat the wound before attempting to treat the fracture.
- NOTE
- Treatment of the fracture depends partly upon the location of the break.
If the fracture is in the upper part of the arm near the shoulder, place a pad or folded towel in the armpit, bandage the arm securely to the body, and support the forearm in a narrow sling.
If the fracture is in the middle of the upper arm, you can use one well-padded splint on the outside of the arm. The splint should extend from the shoulder to the elbow. Fasten the splinted arm firmly to the body and support the forearm in a narrow sling, as illustrated.
Another way of treating a fracture in the middle of the upper arm is to fasten two wide splints (or four narrow ones) about the arm and then support the forearm in a narrow sling. If you use a splint between the arm and the body, be very careful that it does not extend too far up into the armpit; a splint in this position can cause a dangerous compression of the blood vessels and nerves and may be extremely painful to the victim. If the fracture is at or near the elbow, the arm may be either bent or straight. No matter in what position you find the arm, DO NOT ATTEMPT TO STRAIGHTEN IT OR MOVE IT IN ANY WAY. Splint the arm as carefully as possible in the position in which you find it. This will prevent further nerve and blood vessel damage. The only exception to this is if there is no pulse on the other side of the fracture (relative to the heart), in which case gentle traction is applied and then the arm is splinted. Treat the victim for shock and get him under the care of a medical professional as soon as possible.
10b
There are two long bones in the forearm, the radius and the ulna. When both are broken, the arm usually appears to be deformed. When only one is broken, the other acts as a splint and the arm retains a more or less natural appearance. Any fracture of the forearm is likely to result in pain, tenderness, inability to use the forearm, and a kind of wobbly motion at the point of injury. If the fracture is open, a bone will show through. If the fracture is open, stop the bleeding and treat the wound. Apply a sterile dressing over the wound. Carefully straighten the forearm. (Remember that rough handling of a closed fracture may turn it into an open fracture.) Apply two well-padded splints to the forearm, one on the top and one on the bottom. Be sure that the splints are long enough to extend from the elbow to the wrist. Use bandages to hold the splints in place. Put the forearm across the chest. The palm of the hand should be turned in, with the thumb pointing upward. Support the forearm in this position by means of a wide sling and a cravat bandage (see illustration). The hand should be raised about 4 inches above the level of the elbow. Treat the victim for shock and evacuate as soon as possible.
10c
The figure-eight bandage is used for dressings of the ankle, as well as for supporting a sprain. While keeping the foot at a right angle, start a 3-inch bandage around the instep for several turns to anchor it. Carry the bandage upward over the instep and around behind the ankle, forward, and again across the instep and down under the arch, thus completing one figure-eight. Continue the figure-eight turns, overlapping one-third to one-half the width of the bandage and with an occasional turn around the ankle, until the compress is secured or until adequate support is obtained.
10d
Carefully straighten the injured limb. Immobilize the fracture by placing a padded board under the injured limb. The board should be at least 4 inches wide and should reach from the buttock to the heel. Place extra padding under the knee and just above the heel, as shown in the illustration. Use strips of bandage to fasten the leg to the board in four places: (1) just below the knee; (2) just above the knee; (3) at the ankle; and (4) at the thigh. DO NOT COVER THE KNEE ITSELF. Swelling is likely to occur very rapidly, and any bandage or tie fastened over the knee would quickly become too tight. Treat the victim for shock and evacuate as
11
11a
Head wounds must be treated with particular care, since there is always the possibility of brain damage. The general treatment for head wounds is the same as that for other fresh wounds. However, certain special precautions must be observed if you are giving first aid to a person who has suffered a head wound.
- NEVER GIVE ANY MEDICINE.
- Keep the victim lying flat, with the head at the level of the body. Do not raise the feet if the face is flushed. If the victim is having trouble breathing, you may raise the head slightly.
- If the wound is at the back of the head, turn the victim on his or her side.
- Watch closely for vomiting and position the head to avoid getting vomit or saliva into the lungs.
- Do not use direct pressure to control bleeding if the skull is depressed or obviously fractured.
11b
Internal soft-tissue injuries may result from deep wounds, blunt trauma, blast exposure, crushing accidents, bone fracture, poison, or sickness. They may range in seriousness from a simple bruise to life-threatening hemorrhage and shock.
Visible indications of internal soft-tissue injury include the following:
- Vomiting or coughing up bright red blood.
- Excretion of tarry black stools.
- Excretion of bright red blood from the rectum.
- Passing of blood in the urine.
- Nonmenstrual vaginal bleeding.
- Nosebleed.
- Pooling of the blood near the skin surface.
More often than not, however, there will be no visible signs of injury, and you will have to infer the probability of internal soft-tissue injury from other symptoms such as the following:
- Pale, moist, clammy skin.
- Subnormal temperature.
- Rapid, feeble pulse.
- Falling blood pressure.
- Tinnitus (ringing in the ears).
- Fainting.
- Dehydration and thirst.
- Yawning and air hunger.
First aid’s goal must be to obtain the greatest benefit from the victim’s remaining blood supply. The following steps should be taken:
- Treat for shock.
- Keep the victim warm and at rest.
- DO NOT give the victim anything to drink
- Splint injured extremities.
- Apply cold compresses (ice packs) to identifiable injured areas.
- Transport the victim to a medical treatment facility as soon as possible.
11c
A gunshot wound is a medical emergency and will require treatment at a medical facility.
First, control any bleeding by using the pressure points and by elevating the injured area. Do not try to remove the bullet, it may help a doctor to determine the extent of the injury, and its removal may increase the bleeding. Cut or tear away any clothing covering the wound. Do not pour any liquids into the wound. Wipe any debris away from the wound, but be careful not to wipe it towards the wound - always wipe away from the wound. Cover the wound with a bandage and fasten it securely so that it will not hang on anything during transport or slip off. Reassure the victim and get him to a hospital as soon as possible.
11d
Wounds that involve the eyelids or the soft tissue around the eye must be handled carefully to avoid further damage. If the injury does not involve the eyeball, apply a sterile compress and hold it in place with a firm bandage. If the eyeball appears to be injured, use a loose bandage. (Remember that you must NEVER attempt to remove any object that is embedded in the eyeball or that has penetrated it; just apply a dry, sterile compress to cover both eyes, and hold the compress in place with a loose bandage). Any person who has suffered a facial wound that involves the eye, the eyelids, or the tissues around the eye must receive medical attention as soon as possible. Be sure to keep the victim lying down. Use a stretcher for transport.
Many eye wounds contain foreign objects. Dirt, coal, cinders, eyelashes, bits of metal, and a variety of other objects may become lodged in the eye. Since even a small piece of dirt is intensely irritating to the eye, the removal of such objects is important. However, the eye is easily damaged. Impairment of vision (or even total loss of vision) can result from fumbling, inexpert attempts to remove foreign objects from the eye. The following precautions must be observed:
- DO NOT allow the victim to rub the eye.
- DO NOT press against the eye or manipulate it in any way that might cause the object to become embedded in the tissues of the eye. Be very gentle; roughness is almost sure to cause injury to the eye.
- DO NOT use such things as knives, toothpicks, matchsticks, or wires to remove the object.
- DO NOT UNDER ANY CIRCUMSTANCES ATTEMPT TO REMOVE AN OBJECT THAT IS EMBEDDED IN THE EYEBALL OR THAT HAS PENETRATED THE EYE! If you see a splinter or other object sticking out from the eyeball, leave it alone! Only specially trained medical personnel can hope to save the victim’s sight if an object has actually penetrated the eyeball.
Small objects that are lodged on the surface of the eye or on the membrane lining the eyelids can usually be removed by the following procedures:
- Try to wash the eye gently with lukewarm, sterile water. A sterile medicine dropper or a sterile syringe can be used for this purpose. Have the victim lie down, with the head turned slightly to one side. Hold the eyelids apart. Direct the flow of water to the inside corner of the eye, and let it run down to the outside corner. Do not let the water fall directly onto the eyeball.
- Gently pull the lower lid down, and instruct the victim to look up. If you can see the object, try to remove it with the corner of a clean handkerchief or with a small moist cotton swab. You can make the swab by twisting cotton around a wooden applicator, not too tightly, and moistening it with sterile water.
CAUTION: Never use dry cotton anywhere near the eye. It will stick to the eyeball or to the inside of the lids, and you will have the problem of removing it as well as the original object. - If you cannot see the object when the lower lid is pulled down, turn the upper lid back over a smooth wooden applicator. Tell the victim to look down. Place the applicator lengthwise across the center of the upper lid. Grasp the lashes of the upper lid gently but firmly. Press gently with the applicator. Pull up on the eyelashes, turning the lid back over the applicator. If you can see the object, try to remove it with a moist cotton swab or with the corner of a clean handkerchief.
- If the foreign object cannot be removed by any of the above methods, DO NOT MAKE ANY FURTHER ATTEMPTS TO REMOVE IT. Instead, place a small, thick gauze dressing over both eyes and hold it in place with a loose bandage. This limits movement of the injured eye.
- Get medical help for the victim at the earliest opportunity.
11e
Animal Bites
A special kind of infection that must be guarded against in case of animal bites is rabies (sometimes called “hydrophobia”). This disease is caused by a virus that is present in the saliva of infected animals. The disease occurs most commonly in wild animals, but it has been found in domestic animals and household pets. In fact, it is probable that all mammals are susceptible to it. The virus that causes rabies is ordinarily transmitted by a bite, but it can be transmitted by the saliva of an infected animal coming in contact with a fresh wound or with the thin mucous membrane of the lips or nose. The virus does not penetrate normal unbroken skin. If the skin is broken, DO NOT attempt wound closure.
If rabies develops in man, it is usually fatal. A preventive treatment is available and it is very effective, but only if it is started shortly after the bite. Since the vaccine can be obtained only at a medical treatment facility, any person bitten by an animal must be transferred quickly to the nearest treatment facility for evaluation, along with a complete report of the circumstances surrounding the incident. Remember, prevention is of utmost importance. Immediate local treatment of the wound should be given. Wash the wound and the surrounding area carefully, using sterile gauze, soap, and sterile water. Use sterile gauze to dry the wound, and then cover the wound with a sterile dressing. DO NOT use any chemical disinfectant. All of the animal’s saliva must be removed from the victim’s skin to prevent further contamination of the wound. CAUTION: DO NOT allow the animal’s saliva to come in contact with open sores or cuts on your hands. When a person has been bitten by an animal, every effort must be made to catch the animal and to keep it confined for a minimum of 8 to 10 days. DO NOT kill it if there is any possible chance of catching it alive. The symptoms of rabies are not always present in the animal at the time the bite occurs, but the saliva may nevertheless contain the rabies virus. It is essential, therefore, that the animal is kept under observation until a diagnosis can be made. The rabies treatment is given if the animal develops any definite symptoms, if it dies during the observation period, or if for any reason the animal cannot be kept under observation. Remember that any animal bite is dangerous and MUST be evaluated at a treatment facility.
Insect Bites
Though ticks and leeches are not technically insects, we will deal with them here as if they are. Most of the time insect bites and stings will not require first aid. However, you should be aware that there are many insect-borne diseases including Lyme's disease, Rocky Mountain spotted fever, malaria, yellow fever, bubonic plague, etc. Be on the alert for any sickness following an insect bite, and contact a doctor if you suspect transmission of an insect-borne disease.
First aid is aimed at reducing the discomfort caused by an insect bite or sting and preventing infection:
- Get away from the insects to avoid additional bites or stings.
- For stings, scrape the stinger away - do not use tweezers or otherwise pinch a stinger, as this will cause more venom to be injected into the wound.
- Place an ice pack over the affected area to reduce pain and swelling.
- Apply hydrocortizone, calamine lotion, or make a paste from three parts baking soda and one part water and apply that to the affected area.
- Give the patient an antihistamine such as Benadryl.
- Remove ticks by pulling them straight out with a pair of tweezers. Be careful not to break a tick's mouth parts off beneath the skin. Contact the child's doctor who may ask you to save the tick and bring it in for testing. Do not try to remove a tick by touching it with a hot match head or by covering it with petroleum jelly.
- Do not scratch
- Wash the affected area with soap and water.
11f
Fainting
Fainting is a self-correcting, temporary form of shock. It often is the result of a temporary gravitational pooling of the blood as a person stands up. As the person falls, blood again rushes to the head, and the problem is solved. Usually, the serious problems related to fainting are injuries that occur when falling down from the temporary loss of consciousness. Fainting may be caused by stressful situations.
If a person faints (is feels he is about to faint) do the following:
- Lay victim down
- Elevate feet
- Loosen tight clothing
- Maintain an open airway
Epilepsy
Epilepsy, also known as seizures or fits, is a condition characterized by an abnormal focus of activity in the brain that produces severe motor responses or changes in consciousness. Fortunately, epilepsy can often be controlled by medications. Grand mal (tonic-clonic) seizure is the more serious type of seizure. Grand mal seizures may be - but are not always - preceded by an aura. The victim soon comes to recognize these auras, which allows him time to lie down and prepare for the seizure’s onset. A burst of nerve impulses from the brain causes unconsciousness and generalized muscular contractions, often with loss of bladder and bowel control. The primary dangers in a grand mal seizure are injuries resulting from falls and the convulsions as well as a cessation of breathing. A period of unconsciousness or mental confusion follows this type of seizure. When full consciousness returns, the victim will have little or no recollection of the seizure.
First aid is aimed at preventing the patient from injuring himself or herself. Nothing should be placed between the patient’s teeth for any reason. Never try to restrain a victim during convulsions; however, do not leave them alone.
11g
Heat Exhaustion
Heat exhaustion is the most common condition caused by working or exercising in hot spaces. Heat exhaustion produces a serious disruption of blood flow to the brain, heart, and lungs. This causes the victim to experience weakness, dizziness, headache, loss of appetite, and nausea.
Signs and symptoms of heat exhaustion are similar to those of shock: the victim will appear ashen gray; the skin will be cold, moist, and clammy; and the pupils of the eyes may be dilated (enlarged). The vital (blood pressure, temperature, pulse, and respiration) signs usually are normal; however, the victim may have a weak pulse together with rapid and shallow breathing.
Body temperature may be below normal. You should treat heat exhaustion victims as if they were in shock. Loosen the clothing, apply cool wet cloths, move the victim to either a cool or an air-conditioned area, and fan the victim. Do not allow the person to become chilled. If the victim is conscious, administer a solution of 1 teaspoon of salt dissolved in a quart of cool water. If the victim vomits, do not give any more fluids. Transport the victim to a medical facility as soon as possible.
Heat Stroke
Heat stroke is a less common but far more serious condition than heat exhaustion, since it carries a 20 percent fatality rate. The main feature of heatstroke is the extremely high body temperature, 105º F (41º C) or higher, that accompanies it. In heat stroke, the victim has a breakdown of the sweating mechanism and is unable to eliminate excessive body heat built up while exercising. If the body temperature rises too high, the brain, kidneys, and liver may be permanently damaged.
Sometimes the victim may have preliminary symptoms, such as headache, nausea, dizziness, or weakness. Breathing will be deep and rapid at first, later shallow and almost absent. Usually the victim will be flushed, very dry, and very hot. The pupils will be constricted (pinpoint) and the pulse fast and strong.
When you provide first aid for heat stroke, remember that this is a true life-and-death emergency. The longer the victim remains overheated, the higher the chances of irreversible body damage or even death occurring. First aid treatment for heat stroke is designed to reduce body heat. Reduce body heat immediately by dousing the body with cold water, or applying wet, cold towels to the whole body. Move the victim to the coolest possible place and remove as much clothing as possible. Maintain an open airway. Place the victim on his/her back, with the head and shoulders slightly raised. If cold packs are available, place them under the arms, around the neck, at the ankles, and in the groin. Expose the victim to a fan or air-conditioner since drafts will promote cooling. Immersing the victim in a cold water bath is also effective. Give the victim (if conscious) cool water to drink. Do not give any hot drinks or stimulants. Get the victim to a medical facility as soon as possible. Cooling measures must be continued while the victim is being transported.
Hypothermia
Hypothermia is caused by continued exposure to low or rapidly falling temperatures, cold moisture, snow, or ice. Those exposed to low temperatures for extended periods may suffer ill effects, even if they are well protected by clothing, because cold affects the body systems slowly, almost without notice. As the body cools, there are several stages of progressive discomfort and disability. he first symptom is shivering, which is an attempt to generate heat by repeated contractions of surface muscles. This is followed by a feeling of listlessness, indifference, and drowsiness. Unconsciousness can follow quickly. Shock becomes evident as the victim’s eyes assume a glassy stare, respiration becomes slow and shallow, and the pulse is weak or absent. As the body temperature drops even lower, peripheral circulation decreases and the extremities become susceptible to freezing. Finally, death results as the core temperature of the body approaches 80°F (27°C). The steps for treatment of hypothermia are as follows:
- Carefully observe respiratory effort and heart beat; CPR may be required while the warming process is underway.
- Rewarm the victim as soon as possible. It may be necessary to treat other injuries before the victim can be moved to a warmer place. Severe bleeding must be controlled and fractures splinted over clothing before the victim is moved.
- Replace wet or frozen clothing and remove anything that constricts the victim’s arms, legs, or fingers, interfering with circulation.
- If the victim is inside a warm place and is conscious, the most effective method of warming is immersion in a tub of warm (100° to 105°F or 38° to 41°C) water. The water should be warm to the elbow - never hot. Observe closely for signs of respiratory failure and cardiac arrest (rewarming shock). Rewarming shock can be minimized by warming the body trunk before the limbs to prevent vasodilation in the extremities with subsequent shock due to blood volume shifts.
- If a tub is not available, apply external heat to both sides of the victim. Natural body heat (skin to skin) from two rescuers is the best method. This is called “buddy warming.” If this is not practical, use hot water bottles or an electric rewarming blanket. Do not place the blanket or bottles next to bare skin, however, and be careful to monitor the temperature of the artificial heat source, since the victim is very susceptible to burn injury. Because the victim is unable to generate adequate body heat, placement under a blanket or in a sleeping bag is not sufficient treatment.
- If the victim is conscious, give warm liquids to drink. Never give alcoholic beverages or allow the victim to smoke.
- Dry the victim thoroughly if water is used for rewarming.
- As soon as possible, transfer the victim to a definitive care facility. Be alert for the signs of respiratory and cardiac arrest during transfer, and keep the victim warm.
Frostbite
Frostbite occurs when ice crystals form in the skin or deeper tissues after exposure to a temperature of 32°F (0°C) or lower. Depending upon the temperature, altitude, and wind speed, the exposure time necessary to produce frostbite varies from a few minutes to several hours.
The areas most commonly affected are the face and extremities. The symptoms of frostbite are progressive. Victims generally incur this injury without being acutely aware of it. Initially, the affected skin reddens and there is an uncomfortable coldness. With continued heat loss, there is a numbness of the affected area due to reduced circulation. As ice crystals form, the frozen extremity appears white, yellow-white, or mottled blue-white, and is cold, hard, and insensitive to touch or pressure. Frostbite is classified as superficial or deep, depending on the extent of tissue involvement.
Superficial Frostbite
In superficial frostbite the surface of the skin will feel hard or rubbery, but the underlying tissue will be soft, allowing it to move over bony ridges. On the exposed skin on the neck and face it is common to first notice patches that are white or waxy in appearance. This is evidence that only the skin and the region just below it are involved. Very little information is available in wilderness first aid training on the appearance of mid and dark toned skin that has been exposed to mild or superficial frostbite. General treatment for superficial frostbite is as follows:
- Take the victim indoors, or at a minimum, increase their shelter from the elements.
- Superficial frostbite around the head can typically be reversed quickly by sheltering from the elements with a scarf, hat, or even a gloved hand.
- Rewarm hands by placing them under the armpits, against the abdomen, or between the legs.
- Rewarm feet by placing them in the armpit or against the abdomen of the buddy.
- Gradually rewarm the affected area by warm water immersion, skin-to-skin contact, or hot water bottles.
- Place hot water bottles into a dry sock/glove to avoid overheating skin.
- Never rub a frostbite area.
Deep Frostbite
In deep frostbite, the freezing reaches into the deep tissue layers. There are ice crystals in the entire thickness of the extremity. The skin will not move over bony ridges and will feel hard and solid. The objectives of treatment are to protect the frozen areas from further injury, to rapidly thaw the affected area, and to be prepared to respond to circulatory or respiratory difficulties.
- Carefully assess and treat any other injuries first. Constantly monitor the victim’s pulse and breathing since respiratory and heart problems can develop rapidly. Be prepared to administer CPR if necessary.
- Do not attempt to thaw the frostbitten area if there is a possibility of refreezing. It is better to leave the part frozen until the victim arrives at a medical treatment facility equipped for long-term care. Refreezing of a thawed extremity causes severe and disabling damage.
- Treat all victims with injuries to the feet or legs as litter patients. When this is not possible, the victim may walk on the frozen limb, since it has been proven that walking will not lessen the chances of successful treatment as long as the limb has not thawed out.
- When adequate protection from further cold exposure is available, prepare the victim for rewarming by removing all constricting clothing such as gloves, boots, and socks. Boots and clothing frozen on the body should be thawed by warm-water immersion before removal.
- Rapidly rewarm frozen areas by immersion in water at 100°F to 105°F (38°C to 41°C). Keep the water warm by adding fresh hot water, but do not pour the water directly on the injured area. Ensure that the frozen area is completely surrounded by water; do not let it rest on the side or bottom of the tub.
- After rewarming has been completed, pat the area dry with a soft towel. Later it will swell, sting, and burn. Blisters may develop. These should be protected from breaking. Avoid pressure, rubbing, or constriction of the injured area. Keep the skin dry with sterile dressings and place cotton between the toes and fingers to prevent their sticking together.
- Protect the tissue from additional injury and keep it as clean as possible (use sterile dressings and linen).
- Try to improve the general morale and comfort of the victim by giving hot, stimulating fluids such as tea or coffee. Do not allow the victim to smoke or use alcoholic beverages while being treated.
- Transfer to a medical treatment facility as soon as possible. During transportation, slightly elevate the frostbitten area and keep the victim and the injured area warm. Do not allow the injured area to be exposed to the cold.
12
First, do not touch a person who comes into contact with a live electric wire. If you do, the electricity will also flow through your body, and there will be two victims instead of one. Instead, if you can quickly turn off the power source, do so immediately. If it cannot be turned off quickly, try to knock the wire off with something that does not conduct electricity, such as a shoe (take it off first), a wooden broom handle, or a wooden chair.
Once the victim has been separated from the electric power source, check for breathing. If the victim is not breathing, begin artificial respiration (mouth-to-mouth).
13
In a fire, a person is far more likely to die from smoke inhalation than from exposure to flames. There are two things to remember about smoke: it rises, and if you inhale enough of it, it will kill you. Therefore, if you find yourself in a smoke filled room, get down and crawl. If you can, cover your mouth and nose with a wet cloth to help filter the smoke and keep it from entering your lungs. If water is not available, use a dry cloth - it's better than nothing. Make your way to the door and if it is closed, feel it. If it is hot, do not open it, as this means there is fire on the other side. Try to find another way out such as a window or another exit.
14
With the advent of the cell phone, the most effective way of obtaining help in an emergency is by calling 911. Most cell phones are equipped with a GPS module which allows their location to be pin-pointed by a satellite. The cell phone automatically relays this information to the 911 operator.
However, sometimes a cell phone is either not available, or it is not within range of a cell phone antenna tower. If you find yourself facing an emergency in the wilderness, you may have to attempt to signal aircraft. Three ways of doing that are presented here:
Make a distress signal
Make a distress signal on the ground by piling rocks, branches, or other debris to form large letters spelling "S.O.S." This is the universally recognized signal for help. Try to use materials that contrast with the surrounding environment. In winter, you may be able to stomp an SOS into the snow. Make the letters read from east to west (or west to east) so that the shadows catch the letters better.
Light three fires
You may also light three fires to signal for help. Build them either in a line or in a triangle, and get them good and hot. When you see a rescue plane during daylight hours, add green plant matter to the flames. This should cause thick smoke. Be careful to not extinguish the fire by doing this.
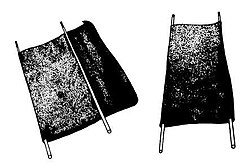
Signaling mirror The emergency signaling mirror is approximately 3 by 5 inches and consists of an aluminized reflecting glass mirror, a back cover glass, and a sighting device. It is used to attract the attention of passing aircraft or ships by reflection, either in sunlight or in hazy weather. The reflections of this shatterproof mirror can be seen at a distance of 30 miles at an altitude of 10,000 feet. Though less effective, and with possible shorter range, mirror flashes can also be seen on cloudy days with limited visibility. To use the mirror, proceed as follows:
- Punch a cross-hole in its center.
- Hold the mirror about 3 inches in front of your face and sight through the cross at the ship or aircraft. The spot of light shining through the hole onto your face will be seen in the cross-hole.
- While keeping a sight on the ship or aircraft, adjust the mirror until the spot of light on your face disappears in the hole. The bright spot, seen through the sight, will then be aimed directly at the search ship or aircraft.
15
15a
The shoulder drag is accomplished by placing the victim in a supine position (laying on his back), grasping the clothing behind his shoulders, and dragging him in the desired direction.
15b
The blanket drag can be used to move a person who, due to the severity of the injury, should not be lifted or carried by one person alone. Place the casualty in the supine position on a blanket and pull the blanket along the floor. Always pull the casualty headfirst, with the head and shoulders slightly raised so that the head will not bump against the floor.
15c
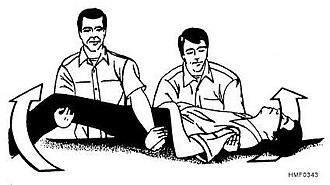
Manual carries are tiring for the bearer(s) and involve the risk of increasing the severity of the casualty’s injury. In some instances, however, they are essential to save the casualty’s life. Although manual carries are accomplished by one or two bearers, the two-man carries are used whenever possible. They provide more comfort to the casualty, are less likely to aggravate his injuries, and are also less tiring for the bearers, thus enabling them to carry him farther.
One two-person carry that can be used in emergencies is shown here. Two rescuers position themselves beside the casualty, on the same side, one at the level of the chest and the other at the thighs. The rescuers interlock adjacent arms as shown, while they support the victim at the shoulders and knees. In unison, they lift the victim and roll his front toward theirs. This carry must not be used to move seriously injured persons.
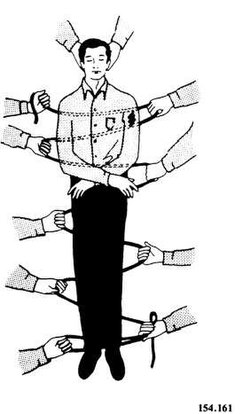
15d
An injured person can be carried by his extremities as shown here. However, this carry should not be used to carry a person who has serious wounds or broken bones.
15e
Standard stretchers should be used whenever possible to transport a seriously injured person. If none are available, it may be necessary for you to improvise. Shutters, doors, boards, and even ladders may be used as stretchers. All stretchers of this kind must be very well padded and great care must be taken to see that the casualty is fastened securely in place. Stretchers may be improvised by using two long poles (about 7 feet or 2.1 meters long) and strong cloth, such as a rug, a blanket, a sheet, a mattress cover, two or three gunny sacks, or two coats. The figure here shows an improvised stretcher made from two poles and a blanket.
CAUTION: Many improvised stretchers do not give sufficient support in cases where there are fractures or extensive wounds of the body. They should be used only when the casualty is able to stand some sagging, bending, or twisting without serious consequences. An example of this type of improvised stretcher would be one made of 40 to 50 feet of rope or 1 1/2-inch firehose.
15f
The three-person hammock carry is very similar to the two-person carry, except that three people are involved: One positioned at the victim's calves, one at the hips, and the third person at the shoulders. The carriers kneel on their knee nearest the victim's feet. The person at the victim's head gives the command, and all three lift the victim to their knees simultaneously. The victim is then turned so that he faces the rescuers. The person at the head then gives the command and the three rescuers stand.
15g
When transporting an injured person, always see that the litter is carried feet forward no matter what the injuries are. This will enable the rear bearer to observe the victim for any respiratory obstruction or stoppage of breathing.